Hypertension
- keoghnicola5
- Jul 20, 2025
- 11 min read
What is Hypertension?
Hypertension, or high blood pressure, is a condition where the force of blood against your artery walls is consistently too high. Whilst hypertension is classified as a medical condition, it could almost be thought of as a risk factor, because if you have someone with high blood pressure, chances are there is already damage done, so cardiovascular disease is already progressing here. So, hypertension is really the output of damage that's already occurring.

Hypertension is characterised by elevated blood pressure over the normal values of 120/80mm Hg in an adult over 18 years of age. This elevation of blood pressure can be divided into three classes of blood pressure:
Class 1-Prehypertension: describes blood pressure measurements of greater than 120mm Hg systolic or 80mm Hg diastolic and less than 130mm Hg systolic or 90mm Hg diastolic. Persons exhibiting prehypertension are encouraged to explore lifestyle modifications to lower blood pressure, but blood pressure lowering agents are not generally prescribed without compelling indications.
Class 2-Stage 1 Hypertension: defined by a blood pressure of over 130mm Hg systolic or 90mm Hg diastolic but less than 160mm Hg systolic or 100mm Hg diastolic. Patients with Stage 1 hypertension are also encouraged to make lifestyle modifications, and initial drug therapy may include thiazide-type diuretics, ACE inhibitors, calcium channel blockers, beta-blockers, and angiotensin-receptor blockers, or a combination of these.
Class 3-Stage 2 Hypertension: defined by a blood pressure greater than 160mm Hg systolic or 100mm Hg diastolic. Persons with Stage 2 hypertension are encouraged to make lifestyle modifications. Two-drug combination therapies (of thiazide-type diuretics, ACE inhibitors, calcium channel blockers, beta-blockers, and angiotensin-receptor blockers) are indicated for these patients.
Understanding the blood pressure monitor
The top/first reading on the monitor is the Systolic blood pressure reading. This measures the pressure in your arteries when your heart beats and pumps blood. It is the force that drives blood out of the heart.
The bottom/second reading on the monitor is the Diastolic blood pressure reading. This measures the pressure in your arteries when your heart is at rest between beats. It is a period of relaxation when the heart fills with blood.
Some monitors may have a pulse oximeter too, usually at the bottom of the monitor with a heart symbol beside it. This measures the heart rate, which is given in units of beats per minute (bpm). These readings vary, depending on the stage of life, activity level, and medication a client may be on, such as beta-blockers, or body temperature.

The three main categories of Hypertension
Primary or essential hypertension: ( 95% )-the most common kind, is idiopathic, and has no single identifiable or medical cause. Drivers include vascular resistance (due to vasoconstriction, atherosclerosis, loss of blood vessel elasticity, increased blood viscosity), obesity, stress & anxiety, smoking, high salt intake, hypercholesterolemia and a family history of high blood pressure.
Secondary hypertension: ( 5% )-results from diseases of the kidneys, adrenals, thyroid, and diabetes. In this type of hypertension, the underlying problem must be treated to reduce the blood pressure. Other known causes of this type of hypertension include sleep apnoea, chronic steroid therapy, Cushing syndrome, and this incidence is higher in men than in women.
Malignant hypertension: also called 'resistant' hypertension, is a hypertensive emergency with extremely high blood pressure. This condition usually results in organ damage, including the central nervous system and the renal system. This is characterised by a diastolic pressure higher than 120 mm Hg, severe headaches, blurred vision, and confusion. May lead to fatal uremia (the build-up of waste products in the blood due to severe kidney dysfunction), myocardial infarction (heart attack), congestive heart failure, or a cerebrovascular accident.
Causes of Hypertension
Genetics: genetic factors are reflected by the fact that African Americans have a higher incidence than do Caucasians and experience a more severe form of hypertension. There are also familial trends, but these reflect lifestyle characteristics as well as heredity.

Obesity: (especially increased abdominal adiposity), which activates a system called the RAAS (renin-angiotensin-aldosterone-system), this is a hormone system which regulates blood pressure but too much activation caused by obesity can activate it to cause too much vasoconstriction and water retention. This system is activated in response to a drop in blood pressure or a decrease in sodium levels in the kidneys, therefore too much activation has the opposite effect of causing high blood pressure.
Excess alcohol: decreases the baroreceptor reflex (a mechanism which has the ability to respond to blood pressure changes). It can also stimulate the sympathetic nervous system, which is responsible for the body's "fight-or-flight" response, causing blood vessels to narrow and the heart to beat faster, both of which increase blood pressure. Electrolyte balance can also be disrupted here, leading to fluid retention and further elevating blood pressure. Long-term, alcohol in excess can weaken the heart muscle and damage blood vessel walls, making it harder for the heart to pump blood effectively and increasing the risk of hypertension.

Stress: prolonged stress causes continuous sympathetic nervous system activity, which causes vasoconstriction (narrowing of the blood vessels) and increased heart rate. Cortisol is a hormone produced by the adrenal glands that sit on top of each kidney, in which levels rise in the blood stream in response to stress. Even though cortisol plays a crucial role in many body functions, including the regulation of blood pressure, it can have a direct impact on blood pressure by causing continuous vasoconstriction if the levels are continuously high, and indirectly affect blood pressure by causing insulin resistance, which is associated with increased risk of hypertension.
Nutritional deficiencies: especially Magnesium, which is a vasodilator (widens the blood vessels), and Potassium, which assists in the urinary excretion of sodium (salt), as sodium can increase blood pressure.
High salt intake: salt-sensitive hypertension is defined as an increase in blood pressure associated with increased salt intake. Approximately 50% of humans with hypertension have salt sensitivity, with this number varying between sexes and influenced by race. Among normotensive individuals (those with normal range blood pressure), approximately 26% are salt sensitive, which has led to increased mortality. Unrefined salts such as Celtic salt are preferrable to table salt as there are trace minerals in unrefined salts, but only to use in moderation.

Inactivity: as we are in a pandemic of inactivity, this is the fourth biggest cause of death worldwide, with 1.4billion people at risk of developing exacerbating chronic illness due to being inactive. All types of physical activity produce blood pressure lowering effects, and improvements are observed for people in every blood pressure category.
Smoking: causes damage to the endothelium (the inner lining of blood vessels)., therefore increasing the chances of developing atherosclerosis (plaque build-up in the blood vessel). Nicotine causes blood vessels to constrict and heart rate to increase, therefore leading to increased blood pressure.
Drugs: long-term use of NSAIDs (non-steroidal anti-inflammatory drugs) contributes to high blood pressure either by antagonizing antihypertensive drugs or by affecting renal function. Other drugs such as corticosteroids and decongestants can also increase blood pressure.
Natural approach to Hypertension

Include fresh fruit and vegetables into your diet daily. A rainbow of fruit and vegetables provides you with lots of different antioxidants, these help to eliminate free radicals from your body (free radicals cause harm to your body if levels are high). The more colours you have the more different ranges of antioxidants, and antioxidants love each other, so you really want to combine them together as they have the capacity to regenerate each other.
Juices such as beetroot juice are a great support for Nitric Oxide, which helps vasodilation of the blood vessels. Also celery juice and parsley are great for the kidneys so assist in excretion of sodium.
These nutrients also help with a good potassium/sodium ratio. Potassium increases natriuresis (removal of sodium to the urine), therefore you are helping to bring down blood pressure. Potassium also lowers sympathetic nervous system activity (sympathetic nervous system activity increases heart rate and blood pressure).
Important information * avoid potassium supplements (get in from your veg), as these can be quite chronic on the gastric system, and can lead to bleeding. Also, if clients are on ACE inhibitor medication for hypertension, these will naturally increase potassium in the body, so adding a supplement too can cause a problem.
DASH diet: (Dietary Approaches to Stop Hypertension). Studies reveal significant systolic and diastolic blood pressure reductions in people with hypertension who have been following this diet.
DASH consists of fresh vegetables and fruits, legumes, nuts, seeds, wholegrains, fish, lean meats, and low-fat dairy, and limits saturated fats and salts. Polyunsaturated/monounsaturated fats are preferred (those found in fish, nuts, seeds), as these can improve overall heart health.
Sodium is also restricted in this diet.
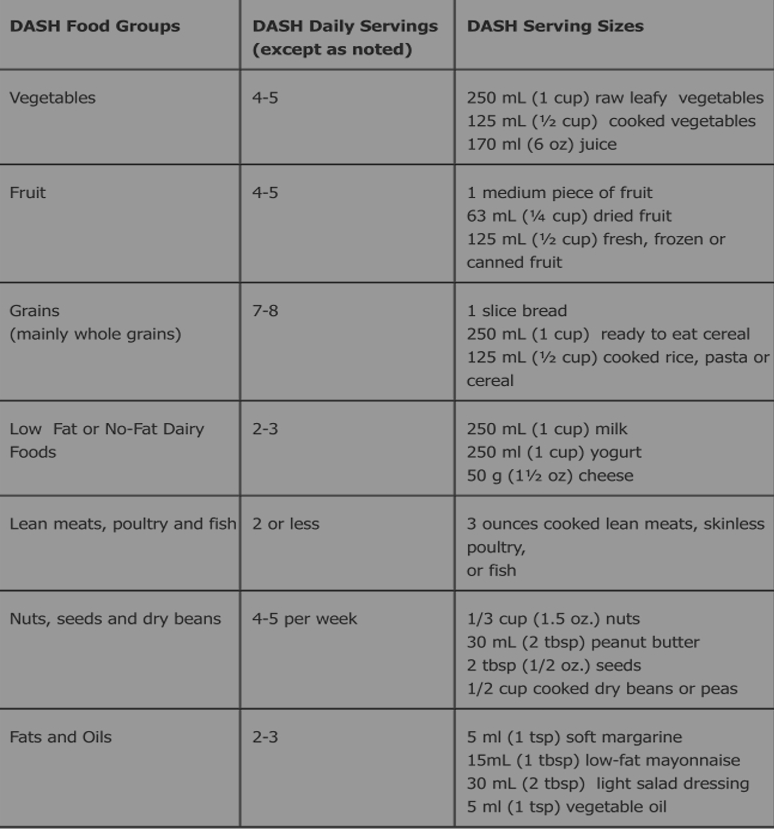
The DASH diet
Optimise sleep: Melatonin is a hormone secreted by the brain during the night, and is associated with anti-hypertensive effects through GABA (Gamma-Aminobutyric Acid) stimulation. GABA is known for producing a calming effect, therefore helping to control anxiety, stress and fear.
Melatonin also is associated with angiotensin II inhibition, a powerful hormone that acts as a vasoconstrictor, narrowing blood vessels.
An increase in Nitric Oxide is also helped by melatonin, which helps to dilate blood vessels, allowing blood pressure to lower.
Weight control: obesity has the capacity to over-activate your blood pressure regulating system (the RAAS, Renin-Angiotensin-Aldosterone System). Within this system you have angiotensin II and aldosterone, which increase blood pressure and blood volume. Angiotensin II directly affects blood pressure by causing vasoconstriction and impacting the pituitary gland to release anti-diuretic hormone, which increases blood volume and blood pressure. It also prompts the adrenal glands to release aldosterone, which prompts the kidneys to increase the reabsorption of water and sodium, increasing blood volume, therefore increasing blood pressure.
Adipocytes (fat cells) secrete hormones which lead to this over-activation of the RAAS.
Control stress: as well as eating a diet rich in nutrients, stress can be supported by other practices such as good sleep hygiene, mindful eating and avoiding caffeine, refined carbohydrates and alcohol, practicing abdominal breathing techniques and supporting the parasympathetic nervous system (rest and digest).
Nutrients to help with Hypertension
Vitamin D: deficiency of vitamin D leads to overexpression of the RAS (renin-angiotensin system), which leads to increased vasoconstriction, and retention of sodium and water.
It also decreases proinflammatory cytokines (signalling molecules released from immune cells which cause inflammation), as well as increasing Nitric Oxide (for vasodilation to lower blood pressure), assists with endothelial function (the inner lining of blood vessels) and arterial elasticity (making arteries more flexible for easier transport of oxygen and nutrients to reach organs of the body).
Vitamin D also lowers hs-CRP (high-sensitivity C-Reactive protein) levels, this is a protein produced by the liver in response to inflammation, and lower levels have less promotion of inflammation and premature disposal of hypoxic cells, which could have regenerated given more time.
The lower the levels of Vitamin D, the higher the risk of hypertension.
Vitamin D food sources: synthesised by the action of sunlight on the skin, fish liver oils-cod, halibut, herring, tuna, butter, egg yolk, milk, sprouted seeds.
Magnesium: deficiency is associated with Hypertension. Alterations in intracellular (within cells) or extracellular (outside cells) magnesium affects cardiac and vascular tone and reactivity, by relaxing the blood vessels and reducing resistance.
Magnesium food sources: almonds, barley, cashews, cocoa, cod, eggs, figs, kelp, leafy greens, legumes, lima beans, mineral water, molasses, parsnips, seeds, soy beans, wholegrain cereals.
L-arginine: Arginine is the principle substrate for vascular Nitric Oxide synthesis. It also helps to modulate the RAS, inhibits ACE activity (angiotensin converting enzyme) which prevents angiotensin I converting to angiotensin II, therefore decreasing its effects (angiotensin II narrows your blood vessels and releases hormones that can raise your blood pressure).
Hypertensive patients display high hs-CRP levels, low apelin (this stimulates nitric oxide in the endothelium, in which it plays a part in lowering blood pressure), and they also have increased arginase (this breaks down arginine). Therefore it is important to include L-arginine in the diet here.
L-arginine food sources: almonds, barley, beans, Brazil nuts, chocolate, dairy products, garlic, ginseng, lactalbumin, peanuts, peanut butter, peas, pecans, raisings, soy protein, sea food, whey, whole wheat.
Vitamin B6: B6 deficiency is associated with hypertension. It can be reduced with someone taking diuretics as these increase the excretion of B6. It is an important co-factor for over 100 enzyme-catalysed reactions in the body, including many which are involved in the synthesis (production of a substance from simpler materials) or catabolism (the breakdown of larger molecules essential for maintaining energy balance) of neurotransmitters.
Increases cysteine synthesis from its storage form which is glutathione (cysteine may exert antihypertensive effects). B6 also blocks Ca (Calcium) channels-when a calcium influx affects our calcium channels in our arteries, it causes vasoconstriction, which causes an increase in our blood pressure.
Get in touch for more advice!
There are many ways to help you to manage hypertension. It is important to understand that there is no one size fits all approach here, as each individual has lots of different areas in their day to day living which may be a cause for their rising blood pressure.
It is also important to have a full investigation into a person's nutrition and lifestyle practices to apply changes naturally where possible before taking supplements or applying practices which may harm or actuate other conditions.
If you need advice on making changes to areas in your life to help with hypertension contact Nicola Keogh Nutrition at www.nicolakeoghnutrition.com or call 0872334990, email keoghnicola5@gmail.com to get booked in now.
References
Mills, KT. Stefanescu, A. He, J. (2020). ‘The global epidemiology of hypertension’. Nat Rev Nephrol. 16(4). 223-237
Poulsen, SB. Fenton, RA. (2019). ‘K+ and the renin-angiotensin-aldosterone system: new insights into their role in blood pressure control and hypertension treatment’. J Physiol. 597(17). 4451-4464.
Bavishi, C. Messerli, FH. Rimold, SF. (2016). ‘Serum Uric Acid in Primary Hypertension From Innocent Bystander to Primum Movens?’.
Cai, W. Duan, X. M. Liu, Y. Yu, J. et al. (2017). ‘Uric Acid Induces Endothelial Dysfunction by Activating the HMGB1/RAGE Signaling Pathway’. BioMed research international. 4391920
Yousefian, M. Shakour, N. Hosseinzadeh, H. Hayes, AW. et al. (2019). ‘The natural phenolic compounds as modulators of NADPH oxidases in hypertension’. Phytomedicine. 1(55). 200-213.
Joshi, S. Ettinger, L. Liebman, SE. (2020). ‘Plant-Based Diets and Hypertension’. American Journal of Lifestyle Medicine. 14(4). 397-Daskaya-Dikmen, C. Yucetepe, A. Karbancioglu-Guler, F. Daskaya, H. et al. (2017). ‘Angiotensin-I-Converting Enzyme (ACE)-Inhibitory Peptides from Plants’. Nutrients. 9(4). 316.
Filippou, CD. Tsioufis, CP. Thomopoulos, CG. Mihas, CC. Dimitriadis, KS. (2020). ‘Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials’. Advances in Nutrition.
Hadi, A. Ghaedi, E. Moradi, S. Pourmasoumi, M. et al. (2019). ‘Effects of Melatonin Supplementation On Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials’. Horm Metab Res. 51(3). 157 164.
Festa, M. Sansone, C. Brunet, C. et al (2020). ‘Cardiovascular Active Peptides of Marine Origin with ACE Inhibitory Activities: Potential Role as Anti-Hypertensive Drugs and in Prevention of SARS-CoV-2 Infection’. International Journal of Molecular Sciences. 21.
Kim, S. Yang, WS. Kim, CH. (2021). ‘Beneficial Effects of Soybean-Derived Bioactive Peptides’. International Journal of Molecular Sciences. 22
Hechtman, L. & Naik, S. (2020). Clinical Naturopathic Medicine. Chatswood, NSW, Churchill Livingstone Elsevier.
Jeon, J. Park, K. (2019). ‘Dietary Vitamin B6 Intake Associated with a Decreased Risk of Cardiovascular Disease: A Prospective Cohort Study’. Nutrients. 11(7). 1484.
Sinatra, ST. Houston, MC. (2022). Nutritional and Integrative Strategies in Cardiovascular Medicine 2nd edition. ISBN 9780367685010. Published May 30, 2022 by CRC Press. 426 Pages 38 Color & 11 B/W Illustrations.
Houston, M. (2013). ‘Nutrition and nutraceutical supplements for the treatment of hypertension: part III’. J Clin Hypertens (Greenwich). 15(12). 931-7.
Cloud, A. (2019). ‘The effect of hawthorn (Crataegus spp.) on blood pressure: A systematic review’. Advances in Integrative Medicine. 7(3). 167-175.
Kanmanthareddy, A. Reddy, M. Ponnaganti, G. Sanjani, HP. et al. (2015). ‘Alternative medicine in atrial fibrillation treatment-Yoga, acupuncture, biofeedback and more’. J Thorac Dis. 7(2). 185-92.
Nalliah, CJ. Sanders, P. Kalman, JM. (2018). ‘The Impact of Diet and Lifestyle on Atrial Fibrillation’. Curr Cardiol Rep. 20(12).137.
Yau, K. & Loke, a. (2021). ‘Effects of diaphragmatic deep breathing exercises on prehypertensive or hypertensive adults: A literature review’. Complement There Clin Pract. 43. 101315
The Nutrient Bible 9th Edition, Henry Osiecki.
Mosby's Dictionary of medicine, nursing & health professionals 11th Edition, Elsevier.
Gould's pathophysiology for the Health Professionals 6th Edition, Robert J. Hubert, Karin C. VanMeter.



Comments